Book Launch: Community Health Practitioners and Child Sexual Abuse in the Family 1970s-2010s - by Ruth Beecher
- Sophie Olson

- Jul 10, 2025
- 6 min read
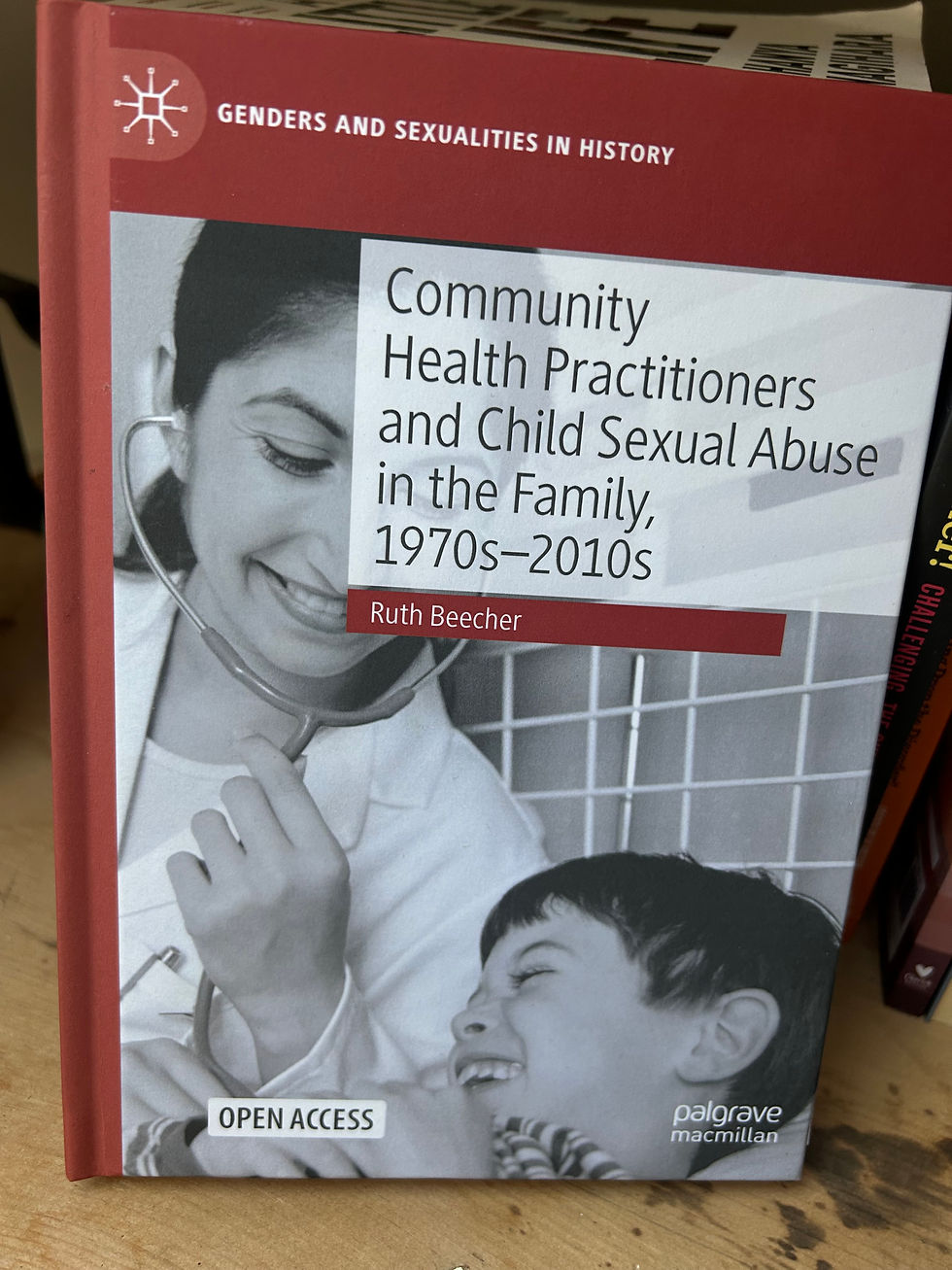
This week I had the privilege of speaking at the launch of Dr Ruth Beecher's new book: Community Health Practitioners and Child Sexual Abuse in the Family, 1970s-2010s - which I’m proud to have endorsed. The book is "an innovative history of community health practitioners’ responses to the seemingly intractable problem of men (and on rare occasions, women) sexually abusing children within the private family home. It is situated within a social history of the development of British community-based health professions in the last decades of the twentieth century."
I joined a brilliant panel chaired by Tanya Serisier, alongside Tracey Loughran, Deborah Hodes and - of course the fantastic Ruth - each bringing valuable and diverse insights to the discussion.
Afterwards I was particularly encouraged to continue the conversation with colleagues around the complex links between child sexual abuse and physical health, in the less understood or medically unexplained conditions that affect the day to day life, of many survivors, including myself eg: CFS, scoliosis, migraines and chronic pain.
I am thankful to Ruth for this brilliant work, and the skillful way she has pulled threads of history together in this relevant and accessible book that should be read by every single practitioner in trauma, health and care. Thank you to everyone involved in creating the event.
I don't usually share my talks outside of events, but for this blog, I feel it might be of benefit. It is slightly adapted from the talk delivered at the launch. Thank you for reading. (Content: Child sexual abuse. Rape. Self Injury. Suicide. Bulimia).
I am a survivor of intrafamilial child sexual abuse - and much of my own experience in terms of the practitioner response - inadequate at best and harmful at worst, is mirrored in Ruth’s book.
My family was middle-class and considered 'privileged'. The man who sexually abused me within my family was a respected pillar of the community, and my signs of abuse were denied, and dismissed. The intersectionality of class and child sexual abuse is still not adequately addressed, and I believe class is a significant barrier to speaking out, which of course plays into the myths of it happening to a certain 'type' of family.
I self-harmed from seven to cope with feelings I couldn’t name. My first rape was at nine. My first (unknown) suicide attempt at fourteen. And through it all, I was off the radar of social services, dismissed by professionals. Once he left the family home, the encouragement was not to speak of him.
Initially I believed I’d shown no signs of child sexual abuse - that I was quiet, well behaved - certainly a day dreamer at school, and yet when I tracked down an old teacher years later, he recalled me as 'troubled, nervous and cowering'. When I asked him if he had raised concerns, he said, “What could I have done?”
So I became a bit of a detective to my own life - because I wanted to understand what had been seen, and dismissed and what other missed opportunities for intervention and support there had been.
Physical proof for me now seems impossible to demonstrate and yet as a child I had UTI’s and soreness - with near constant self-soothing that I wonder, if I was a child today, whether this would be misinterpreted or explained away as 'sensory' or 'neurodivergence'. Another professional saw me self-soothing and she went bright red. She also looked the other way from this behaviour she saw as what? Sexually inappropriate behaviour? - all I know is that I was in pain, and her reaction exacerbated my intense feelings of shame.
In my own book - The Flying Child - A Cautionary Fairy Tale For Adults, I document how it felt to be living in a child’s body that was subject to such abuse, and how I relate child sexual abuse to physical ailments and conditions, from regular chronic nosebleeds in childhood requiring emergency cauterisation, severe headaches, chronic fatigue syndrome leading to me missing nearly a year of school, to the onset of idiopathic scoliosis at 11 years old. None of this has been linked to child sexual abuse by medical practitioners, as conversations like these just don’t happen. ‘No known cause’ is the best they can give me.

Many survivor friends of mine are chronically ill, dying, or died young. Child sexual abuse - of course - is not on their death certificate. My own (degenerative) scoliosis affects my heart and lung function. I have osteopenia in my pelvis and lower spine, and arthritis. Without surgery that is inaccessible to me as I require a trauma informed team that I have been unable to find, I have been told my condition is life-limiting. I can't access pain medication as I find the trauma of medical consultation too much to bear. I can't access dental care, cancer screening, help for menopause, eye tests... I don't know the name of my GP.
I am not a 'complex' patient. I am an invisible one. And we must consider - how many others are there like me? All survivors will have an individual level of tolerance, and not all survivors of child sexual abuse will find medical care retraumatising, but there are only so many times that someone can be retraumatised by a system, before the door to care, closes.
I have come to some level of acceptance about my physical health - but only through necessity. I would rather stay alive. I have four children. I am only 48. This book highlights that had the practitioner response been different when I was a child - I might have had a chance of living a life without these challenges that - lets face it, sometimes make me wonder - is it even a life worth fighting for? My pain levels are intolerable. My physical prognosis is pretty grim.
I digress...
By the time I reached adulthood, my body carried the trauma of child sexual abuse. Chronic pain, severe spinal damage, a broken sense of self. I self-medicated with drugs and alcohol. Bulimia. Food control. I tried university but was thrown out when I couldn’t keep up. Nobody asked why I was struggling. There was no curiosity and no opportunity for conversation.
As a trainer I ask this same question - to practitioners:
"Would you bring child sexual abuse into the conversation?" and the majority say: "No - It's not my job" ('Not My Job' is covered in chapter 7 of this book).
And the same reasons come up every time: lack of training, fear of getting it wrong, lack of time unresolved trauma of the professional - and so on - but underneath we cannot ignore the societal stigma and how being professional doesn’t make us immune to it. And how stigma builds a wall between the child and the support they need.
Every single professional who crossed paths with me, including health practitioners, looked the other way.
And the impact continued…
I spent years trapped in a mental health system that treated my trauma as illness, eventually being told by a psychiatrist I would 'never recover'. I was harmed again when I tried to disclose to my consultant, to give more context to my survival mechanisms he saw as 'symptoms'. He invited my birth family into the hospital for a forced disclosure, and I tried to take my own life as a result.
He then terminated the doctor/patient relationship saying there was nothing more he could do for me.
What I have found both unsurprising and disturbing about Ruth’s book, is the fact that there is such uniformity and similarity across survivor testimony. What is even more worrying is that, historically, not a lot seems to have changed or improved. We have had public outrage, followed by independent inquiries, yet the outcomes for survivors of sexual abuse are, on the whole, startlingly familiar to those of us who share these experiences.
For me, the hope in this book lies in provided examples of the ways that certain individual health practitioners did make themselves accessible to children, despite a lack of vision and leadership within their professions. This is also thankfully something I can relate to, as I found a practitioner like this but it shouldn’t have taken 40 years.
The most important question, and one I believe can influence change in all sectors (not just healthcare), is asked by Ruth directly;
“Can these individual examples of allyship be transformed to a stronger collective everyday practice?”
I believe the answer is yes - but it requires the allies to drive it as much as the victim/survivors to need it.
Community Health Practitioners and Child Sexual Abuse in the Family, 1970s-2010s by Ruth Beecher is an open access book and you can find more about it here.



Comments